Frozen Shoulder & OTZ
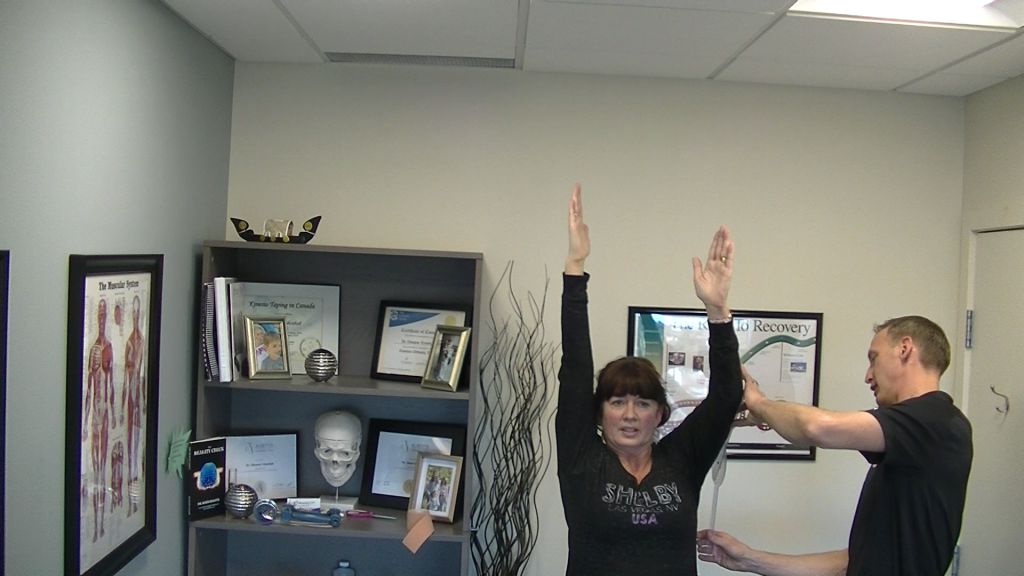
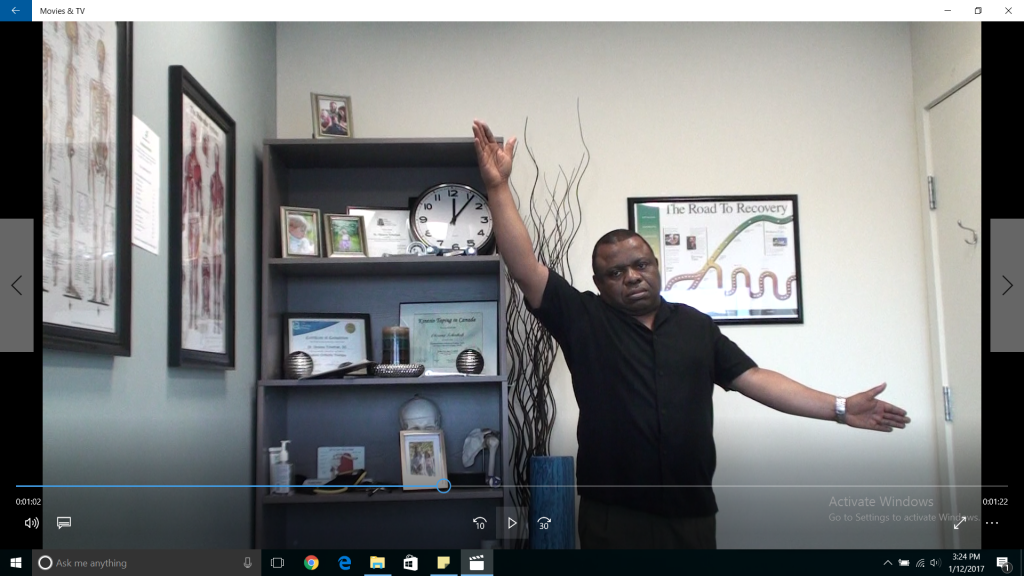
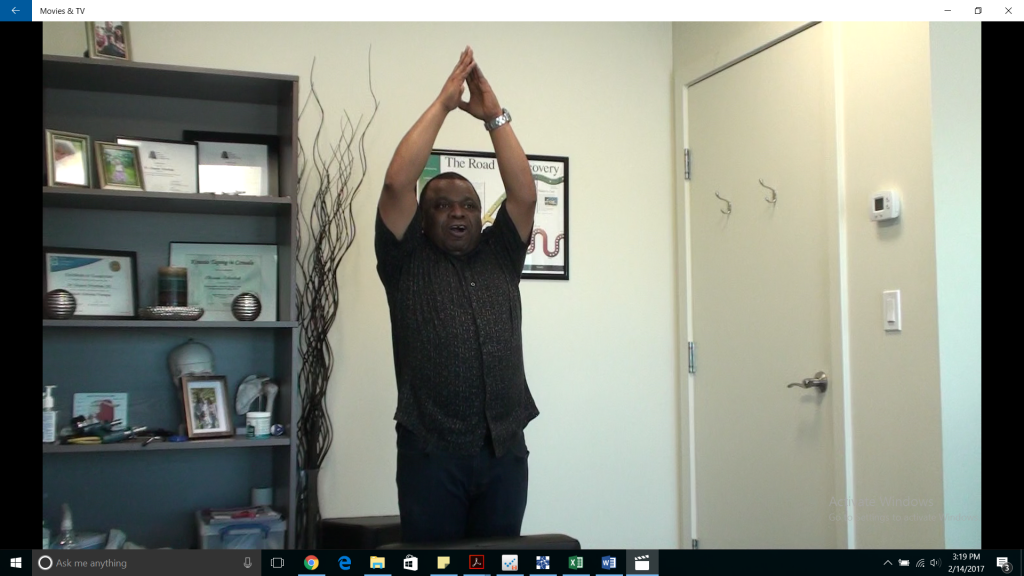
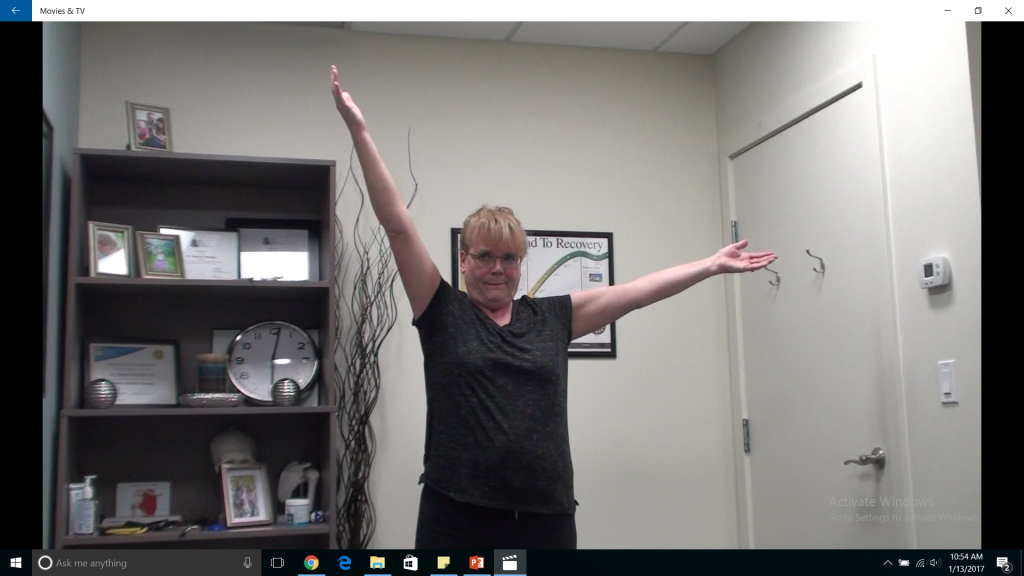
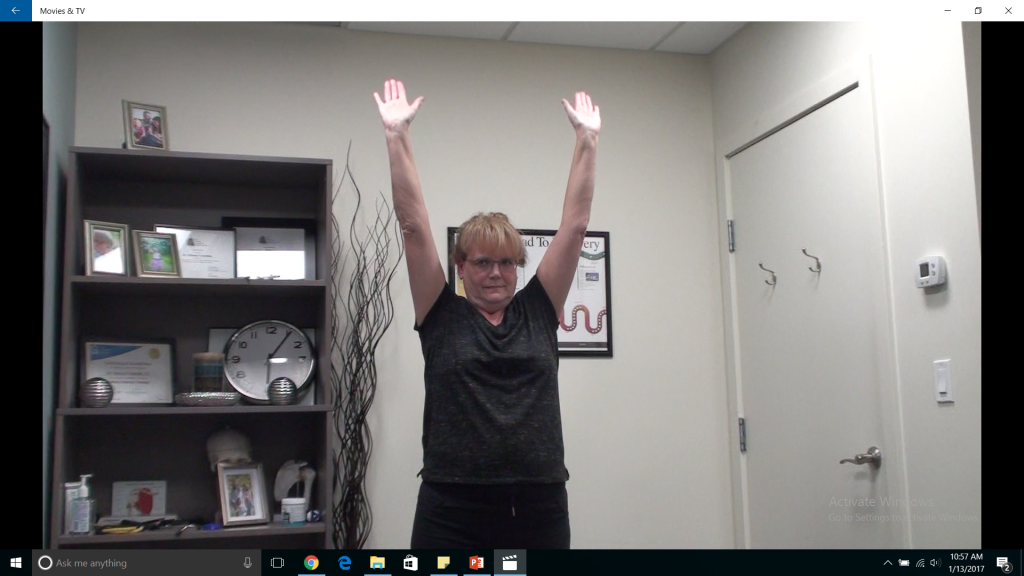
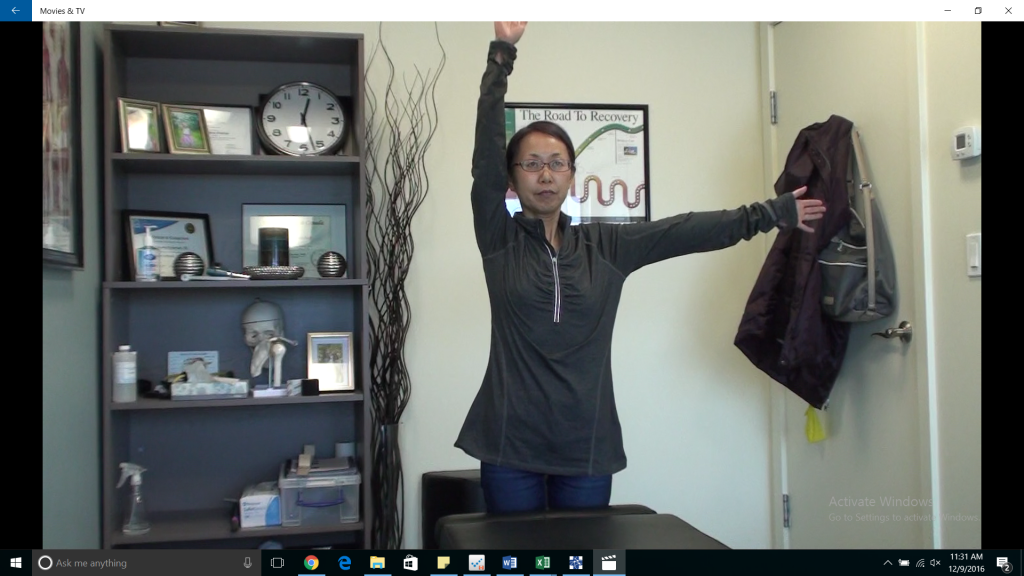
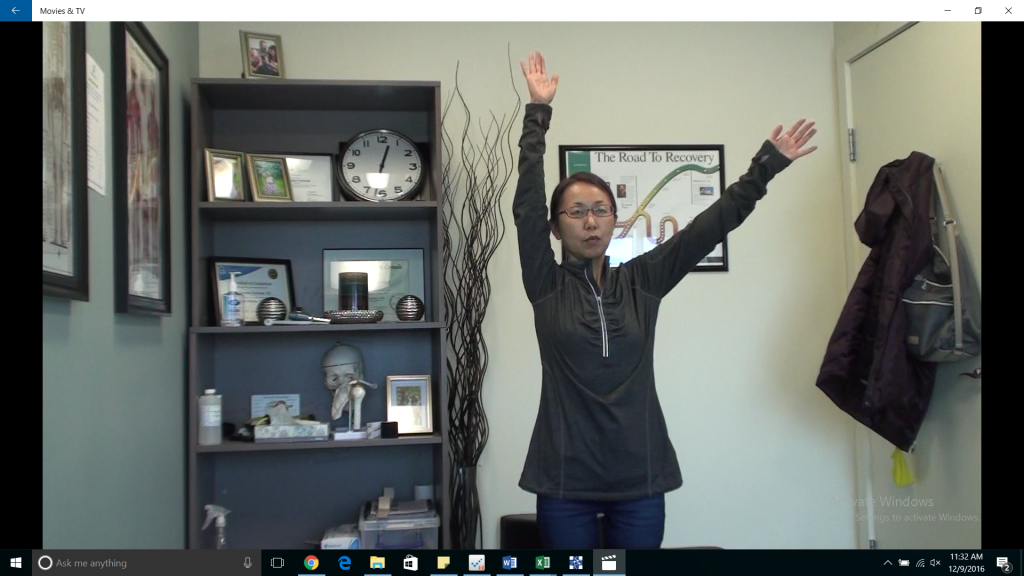
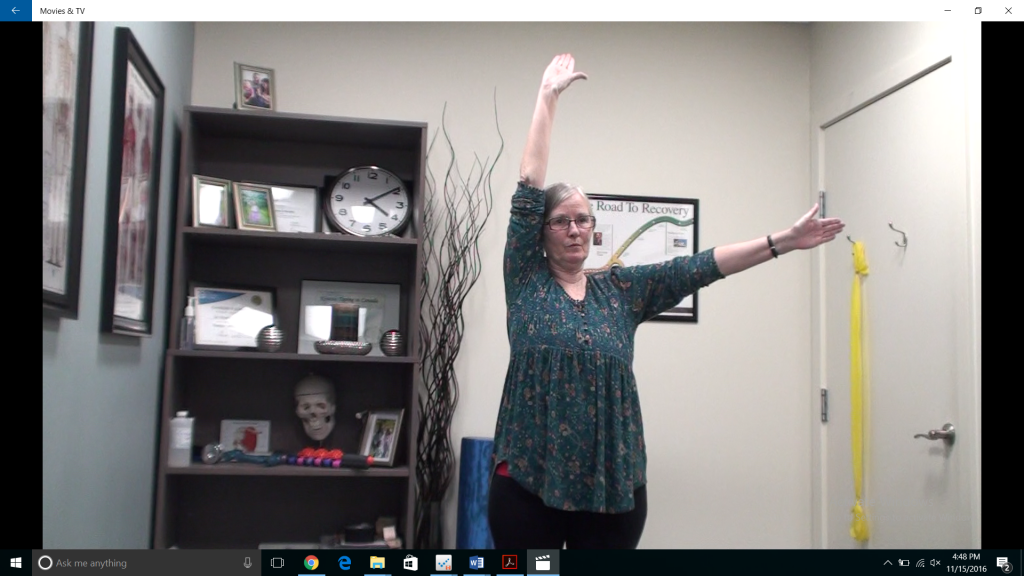
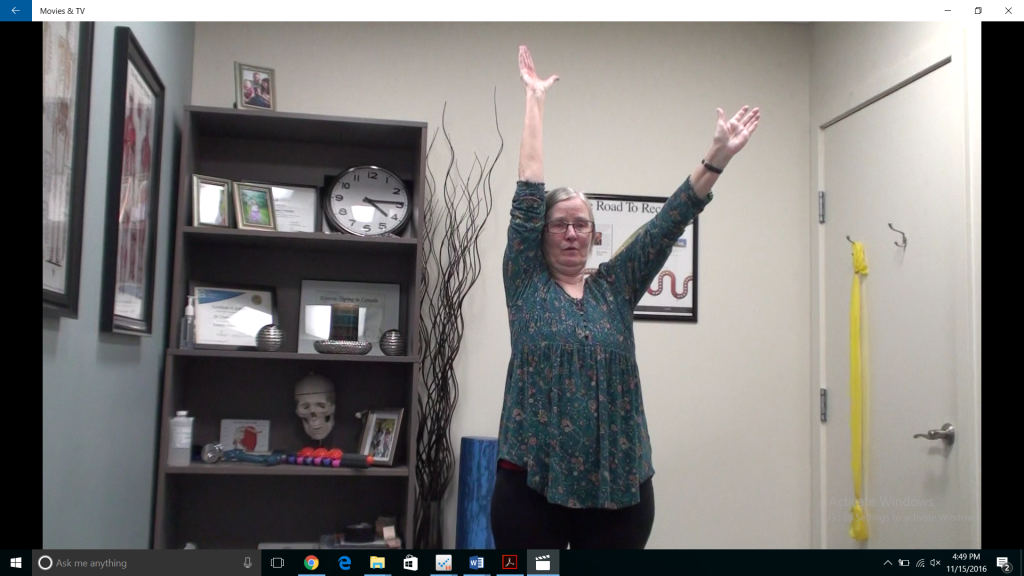
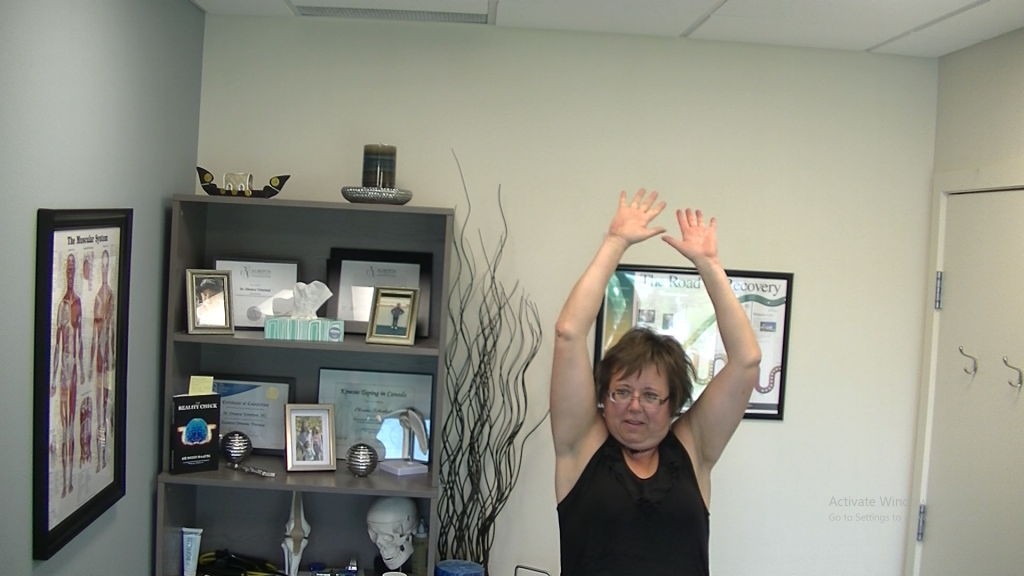
Actual patients. Pre and post treatment.
Frozen Shoulder/Adhesive Capsulitis

|
Traditional Treatments for Adhesive Capsulitis/Frozen Shoulder:
Western Medicine categorizes and treats this condition as a physical joint problem where the limitation in shoulder range of motion is due to scar tissue (adhesions) building up in the shoulder joint. This is why the condition is called “Adhesive capsulitis” of the shoulder. It is important to point out that Frozen Shoulder is considered an ” idiopathic “condition, meaning it is not understood how or why it happens.
Traditional treatments fall into four categories that are sometimes combined. Patients often progress through these treatments as their condition becomes more chronic and other modalities fail. The types of treatment are: watchful waiting, physiotherapy/manual therapy with NSAID therapy, corticosteroid injections and finally surgical procedures. These traditional treatments can be extremely painful (physiotherapy and manual therapy, surgical recovery), frustrating and may weaken the joint or cause further injuries (corticosteroid shots, surgical procedures) 1 (E Maund, 2012). To add to an “adhesive capsulitis” patient’s dilemma, these treatments have mixed results and often have little or no effect in reducing the duration and severity of the frozen shoulder. The majority of cases self-resolve in a similar time period with or without treatment 3,2.
In other words, after significant expense and enduring much suffering treating this condition, the patient often finds themselves no further ahead.
A NEW IDEA, INTRODUCING OTZ:
In the world of chiropractic, there is a new and innovative concept for treatment of this stubborn and clinically frustrating condition. Rather than the traditional Orthopedic, or physical joint model of Frozen Shoulder, a Texas chiropractor (Dr. Francis Murphy) has proposed a Neurological Model for the cause of Frozen Shoulder. He named the corresponding treatment technique OTZ, which stands for One To Zero and reflects the on/off nature of neurons. Using the OTZ based treatments, many FSS patients are getting significant, effective and often immediate, and lasting relief.
The Big Picture. How does the OTZ approach work? :
(If the following description is too general, please scroll to the bottom of the page for a description of the mechanism in more technical terms suitable for healthcare professionals.)
After trauma or as a result of chronic postural changes, the skull and the upper neck lose their normal neutral position and normal motion. These changes, and other postural changes in the upper thoracic and cervical spines, affect the function of certain important neurological structures. Among these neurological structures is the Spinal Accessory Nerve. This nerve is vital to coordinate efficient and healthy motion of the same side shoulder. Specifically, without proper Spinal Accessory Nerve function the shoulder blade and collar bone are no longer able to move and stabilize properly to support proper motion of the arm. As a result, the shoulder has great difficulty rising above 90 degrees in abduction or being significantly internally or externally rotated. This reduced neurological function coupled with the postural changes results in chronic inflammation in the shoulder and damage to the internal tissues of the shoulder (capsule, labrum, rotator cuff). Reduced range of motion, accumulation of scar tissue, and pain typical of adhesive capsulitis/FSS is the result.
The OTZ upper cervical adjustment acts to restore biomechanical function in the upper cervical spine and removing or reducing the impact on the Spinal Accessory Nerve. By correcting this specific dysfunction, the vital link between the brain and the muscles that coordinate shoulder function is restored. Range of motion and pain levels are often dramatically and immediately improved. Patients will usually have to undergo postural rehabilitation in conjunction with the specific OTZ adjusting protocols to achieve complete recovery.
| The OTZ adjustment, can anybody do it?
The adjustment for the specific dysfunction in the upper neck that leads to Frozen Shoulder Syndrome is a very specific and precise procedure. It should only be performed by a licensed chiropractor. Your chiropractor or Youtube may make it look easy, but please don’t attempt this at home. The structures in this area of the upper neck are very sensitive and important. As such, proper training is absolutely necessary. If you or someone you know is potentially suffering from FSS, contact Dr. Denis Simons to arrange a consultation and determine if you/they are a good candidate for the OTZ procedure. |
1 E Maund, D. C. (2012). Management of frozen shoulder: a systematic review and cost effectiveness analysis. Health Technology Assessment.
2 Filip Struyf, M. M. (Dec 2013). Current evidence on physical therapy in patients with adhesive capsulitis: what are we missing? Clinical Rheumatology.
3 LORI B. SIEGEL, M. N. (1999). Adhesive Capsulitis: A Sticky Issue. American Family Physician
|
Technical description of proposed mechanism of action: While adhesions are often present in cases of Frozen Shoulder Syndrome, if the proposed mechanism is correct, they are secondary to impaired neurological control and mechanical position of the shoulder. The proposed theory recognizes that most cases of FSS are complex and multi-factorial but suggests the impaired function of Cranial Nerve XI (CN XI), is a significant factor in the development of FSS. CNXI is the pathway by which the brain activates and controls the trapezius and SCM muscles. The trapezius muscle controls, positions and dynamically stabilizes the shoulder blade ipsilaterally (same side) to allow certain types of motion. Without coordinated action of this muscle on the scapula, motion of the humerus into abduction above 90 degrees and into external rotation is impeded by contact of the humerus and acromion (part of the scapula). This nerve is vulnerable to dysfunction in the upper cervical spine because of its unique path. Rather than originating in the cranium like other Cranial Nerves, the spinal rootlets for CN XI exit the spinal cord between the 1st and 5th cervical levels and then ascend within the spinal canal through the foramen magnum. Once in the skull, the spinal root of CN XII joins it’s cranial root and exits the cranium via the jugular foramen with cranial nerves IX and X. It’s this route up through the foramen magnum passing between the brainstem and the skull and all of the other associated structures that makes it vulnerable to compression or potentially tethering/traction. |
 |
| Patients with frozen shoulder typically display a subtle contra-lateral flexion/ipsilateral rotation extension head posture coupled with a flattening of the normal cervical lordosis and anterior translation of the occiput on the atlas. These postural changes can negatively impact the function of CN XI in one of two ways. The spinal root of the cranial nerve can either be directly compressed at the level of the foramen magnum as the skull becomes fixed anteriorly, or the straightening of the cervical curve coupled with an ipsilateral lifting of the occiput as it slides laterally and superiorly on the superior articular facet of C1 can generate a tethering effect on the cervical cord. In the latter mechanism, other cranial nerves may be impacted (typically between CN VIII and XII), and the patient may exhibit other chronic symptoms of the ipsilateral upper extremity (chronic epicondylitis, hypoperfusion, carpal tunnel like symptoms, etc.). Dr Murphy named these specific postural distortions the Hatcher Murphy Subluxation (HMS) and they can be objectively observed with postural and physical examinations and confirmed with radiological examination. As a result, the OTZ method involves a detailed radiological, physical, postural and cranial nerve examination.
If these postural and biomechanical changes are found, and contra-indications to treatment are not present, a specific chiropractic adjustment is applied to reduce this biomechanical distortion. When applied correctly to the upper cervical spine, these distortions are reduced improving vital neurological functions and many patients experience immediate and dramatic reductions in pain with significant increases in active shoulder and neck range. Patient’s that have successful outcomes with this combined chiropractic and postural rehabilitation treatment typically experience significant results in the first few treatments. |
|









44 thoughts on “Frozen Shoulder & OTZ”
Comments are closed.